Direct Bilirubin: Normal Range, High Levels, and Causes Explained
Time to read 11 min
Time to read 11 min
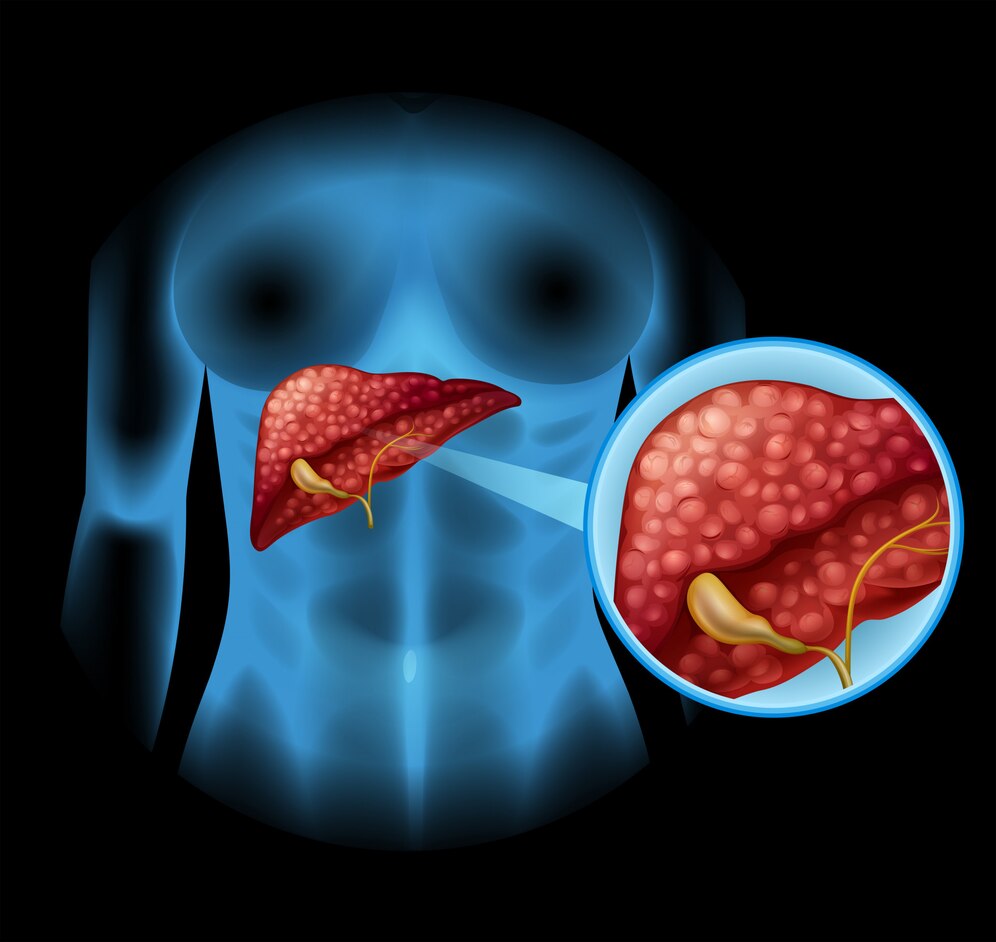
The body depends on direct bilirubin for both breaking down blood proteins and removing waste through the elimination pathway. This compound dissolves in water, which enables the liver to process it before bile elimination occurs. Direct bilirubin elevations in bilirubin in your blood indicate the presence of liver dysfunction or bile duct obstruction or any hepatic conditions.
Direct bilirubin measurement accuracy stands vital for liver disease diagnosis and monitoring, which transforms it into a crucial testing element in medical practice. The waste elimination mechanism of the body depends significantly on direct bilirubin, which shows indicators for liver malfunction as well as bile duct blockages and alternative medical conditions.
Blood test direct bilirubin analysis plays a crucial role in liver function evaluation and diagnosing both hepatic and biliary medical conditions. The efficient breakdown and elimination of bilirubin by the liver depends on direct bilirubin levels, and any irregular levels indicate liver diseases, including hepatitis, as well as liver cirrhosis or bile duct blockage. Medical intervention starts on time because routine blood tests reveal direct bilirubin levels before it is too late. Health professionals need to precisely interpret bilirubin blood test measures because this constitutes an essential aspect of thorough medical investigations and continuous patient health assessments.
Direct bilirubin, also known as conjugated bilirubin, is a form of bilirubin that has been processed by the liver to become water-soluble, allowing it to be excreted through bile into the digestive system. It plays a vital role in the body's ability to remove waste products from the breakdown of red blood cells. Understanding what direct bilirubin is helps in recognizing its importance in bilirubin metabolism, liver function, and in diagnosing potential liver or bile duct issues when levels become abnormal.
The normal quantity of direct (conjugated) bilirubin exists between 0.1 to 0.3 mg/dL for adult individuals. The ranges between 0.1 to 0.3 mg/dL remain essential for normal liver function and waste elimination activities in the body. When direct bilirubin measurement deviates from this normal range, healthcare providers must review cases for liver disease possibilities as well as bile duct obstructions and additional health problems. Medical detection and proper disease management depend on the continuous monitoring of direct bilirubin levels achieved through standard blood testing.
The acceptable normal bilirubin levels for direct bilirubin in blood tests is under 0.2 mg/dL, but small fluctuations may happen based on patient age and medical situation. Newborn bilirubin monitoring is essential because elevated results might reveal either neonatal jaundice or liver immaturity, or more severe underlying medical conditions. Early diagnosis combined with suitable treatments helps avoid kernicterus development and supports normal growth in babies during the essential early stages of development.
High levels of direct bilirubin show that conjugated bilirubin exceeds normal amounts in blood circulation. High direct bilirubin levels develop from medical conditions that impact liver function, bile ducts, and red blood cells. The body shows liver damage or bile duct obstruction when conjugated hyperbilirubinemia, indicated by direct bilirubin values, increases. The main origins of the direct bilirubin increase in blood include:
The liver function gets negatively affected by specific diseases, which prevent proper bilirubin breakdown. The development of either benign or malignant tumors in the liver results in bile flow blockage, which leads to improper bilirubin excretion, thus causing direct bilirubin to build up in the blood circulation.
Elevated direct bilirubin occurs as a result of genetic disorders that impair normal bilirubin metabolic processes. The liver fails to transfer conjugated bilirubin into bile as an inherited medical condition, which remains quite rare. A direct bilirubin accumulation emerges in the bloodstream because of this condition.
Bilirubin cannot depart from the bloodstream to reach the intestines because of blocked bile ducts, which promotes direct bilirubin accumulation. Restrictions within gallbladder stones permit their movement toward the bile ducts until these ducts become blocked and prevent bile from flowing. A malignancy of the bile ducts rarely appears, which prevents bile from flowing normally, thus causing obstructive jaundice accompanied by increased direct bilirubin concentrations.
The specific infections that impact liver functioning ability cause an elevation of direct bilirubin measurements. The death of red blood cells due to malaria parasite activity results in higher levels of bilirubin within the body. A bacterial disease from Leptospira infects the liver through damage and results in elevated direct bilirubin levels.
The presence of toxic substances, including medications along with alcohol can harm liver tissues which results in higher levels of direct bilirubin in the patient's body. Some examples include cardiovascular disease, alcohol abuse as a chronic habit leads to liver problems that result in cirrhosis and inflammation along with jaundice, which increases the levels of direct bilirubin . Alcohol abuse as a chronic habit leads to liver problems that result in cirrhosis and inflammation along with jaundice, which increases the levels of direct bilirubin.
Unconjugated bilirubin increases when red blood cells undergo destruction during the process known as hemolysis. The liver may become unable to manage extreme bilirubin levels when severe hemolysis occurs, thus causing direct bilirubin concentrations to increase.
Among newborns, there exists a birth defect named biliary atresia, which causes malformed or obstructed bile ducts. The obstruction of bile flow leads to conjugated bilirubin accumulation, which appears in blood results from this condition. The treatment approach for biliary atresia requires surgery or liver transplantation after the jaundice presents itself, since the condition remains untreated.
Healthcare providers perform the direct bilirubin blood test for two essential purposes. it examines liver function and investigates bile flow abnormalities. Healthcare providers examine how much conjugated bilirubin exists in blood to identify liver diseases and detect bile duct restrictions and similar health issues. The testing procedure supports both early identification of hepatic problems and swift diagnosis, which enables appropriate treatment and aids in multiple hepatic disorders. Thus, this test serves as vital content in complete healthcare assessments.
Medical tests show high direct bilirubin patterns because the liver processes bilirubin but fails to eliminate it properly, resulting from bile duct obstructions or liver inflammation or hepatocellular damage. Medical attention is needed for immediate evaluation because such increases indicate serious medical conditions. Knowledge about why direct bilirubin increases, as well as its health effects, enables proper diagnosis and successful treatment of liver or biliary system health problems.
Direct bilirubin increases primarily because of liver diseases like hepatitis and cirrhosis, together with bile duct blockage and cholestasis conditions. The liver fails to eliminate conjugated bilirubin because of these medical conditions, which results in the buildup of this substance in the bloodstream. Acceptable diagnosis and proper treatment of elevated direct bilirubin require knowledge of its underlying causes for effective prevention of complications. The outcomes of patients with elevated bilirubin improve when healthcare providers monitor and intervene promptly.
Newborns need direct bilirubin assessment for diagnosing liver and biliary system functionality during infancy. Arising bilirubin levels during early infancy normally adapt to birth, but increased or sustained levels might indicate neonatal conditions like hepatitis or biliary atresia or liver diseases. Newborn direct bilirubin assessment must happen as soon as possible, together with appropriate medical evaluation, because this procedure protects the baby's health and identifies necessary treatment promptly.
Determining the distinction between direct and indirect bilirubin enables healthcare professionals to correctly evaluate liver function and diagnose associated medical disorders. Unconjugated (indirect) bilirubin forms first through red blood cell breakdown, and conjugated (direct) bilirubin represents the processed and water-soluble substance the liver releases into bile. Healthcare providers who understand this difference can diagnose targeted treatment for patients by identifying specific conditions, including hemolytic anemia and liver dysfunction or bile duct obstruction.
An elevated direct bilirubin concentration in blood develops into jaundice and causes yellowing of the skin and the whites of the eyes. When the liver fails to process bilirubin effectively or the bile ducts become obstruction, that stops bilirubin excretion, and jaundice occurs. When bilirubin fails to move through the bile channel, it instead enters the urine stream, leading to a darkened urine appearance. Bilirubin reaching the intestines is necessary for preventing stools from becoming light in color. A high amount of bilirubin results in intense itching because bile salts build up in the skin tissues.
The medical condition known as Kernicterus develops when high bilirubin levels affect newborns in particular, and this leads to a serious complication with rare occurrence. Neurological damage in the brain occurs because the bloodstream lets too much bilirubin reach central nervous system tissue. The condition primarily develops in infant patients who suffer from severe jaundice when their indirect bilirubin measurement exceeds 20 mg/dL. Kernicterus becomes a permanent condition leading to delays in development and cerebral palsy, as well as hearing deficits and vision impairment, when medical treatment does not occur.
LFTS, which includes direct bilirubin testing, allow healthcare providers to check liver processing capacities that affect bilirubin excretion levels. Healthcare providers use the test measures to measure direct bilirubin concentrations in blood because it provides insights about liver function, together with bile flow and liver and biliary conditions. Direct bilirubin measurement is an essential diagnostic tool because it helps health professionals identify jaundice, liver disease, along bile duct obstruction. A medical team needs to monitor patients continuously while interpreting results correctly to properly handle underlying health factors caused by abnormal bilirubin levels.
High direct bilirubin levels might signal the presence of medical issues that affect the liver or gallbladder, or bile ducts. Raised bilirubin levels should always receive medical attention, despite whether these levels indicate immediate danger. The condition suggests hepatitis or bile duct blockage, or liver malfunction, which should be medically assessed and treated properly. Early identification of health problems, together with immediate medical help, is essential for preserving the health of your liver and minimizing serious complications, including abnormal total bilirubin level . Seek immediate medical attention if you show symptomatic indicators of jaundice, including dark urine, together with abnormal test results and abdominal pain.
Direct bilirubin symptoms usually originate from liver or bile duct conditions, but they provide crucial indications of medical problems. The most frequent indications of high direct bilirubin are jaundice, together with dark-colored urine and pale stool appearance and skin itching and exhaustion and discomfort in the abdomen, which may also affect mucus membranes . Direct bilirubin signs must not be ignored because they might suggest liver inflammation or blocked bile ducts, or diseases affecting the gallbladder. An early identification of these symptoms, followed by medical assistance, results in quick diagnosis alongside proper treatment, which helps avoid more severe outcomes.
Individuals with elevated direct bilirubin must treat their specific medical causes, which include liver disease, along with bile duct obstruction or associated medical conditions. Medical care consists of liver inflammation medications, together with bile duct surgery and healthy dietary choices and alcohol avoidance. The prompt medical diagnosis followed by appropriate treatment stands as a critical requirement for both decreasing bilirubin levels and obstructing complications while fostering ideal liver health as well as total health satisfaction. Medical progress needs regular monitoring to ensure appropriate changes in treatment approaches.
A healthy adult population shows direct bilirubin levels between 0.1 to 0.3 mg/dL, since this measurement reflects liver health. An increase in direct bilirubin concentration suggests conditions regarding liver dysfunction or biliary system problems, which include bile duct obstructions and hepatitis and liver cirrhosis. Early diagnosis and proper treatment depend on both knowing normal ranges for direct bilirubin and identifying its possible causes. The practice of keeping bilirubin levels under surveillance helps doctors detect health disorders, including conditions associated with low levels, and deliver suitable treatments for liver care.
The liver's capacity to process bilirubin into direct components or to excrete it turns poor when the liver shows dysfunction through hepatic conditions or bile duct blockage. Medical evaluation for identifying the root cause of elevated direct bilirubin levels becomes essential because these results generate serious concern.
The specific levels of direct bilirubin reflect liver operational status and differ according to age. Adults show normal direct bilirubin measurement when their levels range from 0.1 to 0.3 mg/dL. During infancy direct bilirubin amounts remain lower than 0.2 mg/dL because the liver performs more slowly after birth.
The direct bilirubin measurement of 0.40 mg/dL exists above the typical adult range that spans from 0.1 to 0.3 mg/dL. At this elevated bilirubin level one may suspect liver or biliary medical conditions that show slight liver impairment or early blockage of bile ducts.
Elevated direct bilirubin levels in blood show that there are problems with the liver and biliary systems. The liver cells transform bilirubin derived from red blood cell breakdown into direct bilirubin. Direct bilirubin carries the medical name "conjugated bilirubin."
The path of remedy for elevated direct bilirubin depends entirely on what causes its increase. Treatment for liver-related direct bilirubin elevation requires medication together with lifestyle changes as well as antiviral therapy and immunosuppressant drugs in select cases.
The medical field considers 0.40 mg/dL direct bilirubin normal for most patients since normal values exist between 0.0 and 0.3 mg/dL. The test results may exhibit slight deviations because of laboratory reference range limitations and unique health conditions of patients.
Medical attention becomes necessary when total bilirubin numbers rise above 2.5 to 3.0 mg/dL and when direct bilirubin concentration increases above the other fractions. Doctors should initiate medical intervention as soon as total bilirubin reaches levels above the reported threshold from a blood sample since these elevated results point toward severe liver malfunction or blocked bile ducts or blood cell destruction (hemolysis).
High bilirubin levels in blood tests usually show the possibility of health problems affecting liver function or bile ducts or red blood cells. Elevated bilirubin levels result in jaundice through yellow discoloration of skin and eyes in addition to possible yellow urine color and paler stool appearance and skin itchiness.
**Medical Disclaimer: The following information is for educational purposes only. No information provided on this website, including text, graphics, and images, is intended as a substitute for professional medical advice. Please consult with your doctor about specific medical advice about your condition(s).

