Zonulin
Time to read 7 min
Time to read 7 min
Zonulin is one of the most important regulators of intestinal permeability. For a long time, research has demonstrated that dysregulation of the zonulin pathway has been linked with multiple diseases, particularly those involving chronic inflammation, autoimmunity, and changes to the intestinal barrier function.
The molecular and clinical significance of zonulin, its action mechanism, and disease association such as celiac disease, type 1 diabetes, and inflammatory bowel disease are discussed in this article.
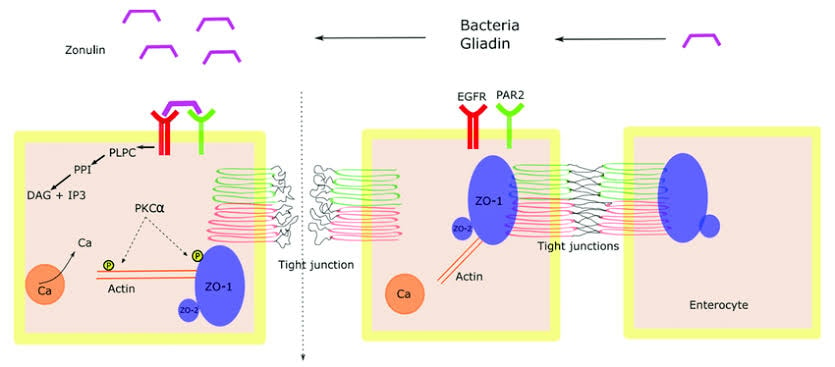
Zonulin is a protein that controls the tight junction permeability of intestinal cells. Tight junctions are specialized structures for selective impedance by the intestinal epithelium.
It allows nutrients and some substances into the bloodstream while keeping others tightly restricted from entering the bloodstream. The regulation of the intestinal barrier is controlled by the zonulin; therefore, any malfunction on this intestinal barrier results in increased intestinal permeability, which is also called "leaky gut.".
The leaky gut concept is a novel idea that has lately been stressed because it has been associated with many inflammatory and autoimmune conditions.
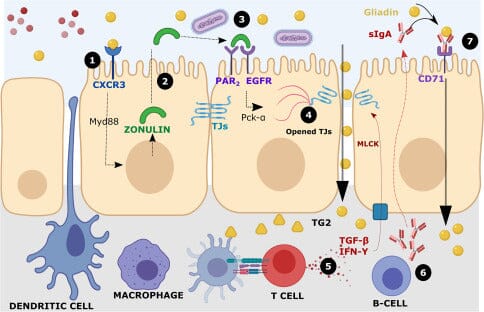
Increased permeability of the intestine allows toxins, antigens, and other macromolecules to pass through the intestinal barrier and cause immune responses that lead to the pathology of diseases.
It has been shown to be released from the epithelial layer in response to certain stimuli, including bacterial colonization or gluten exposure, which increases the permeability of tight junctions.
Increased intestinal permeability might contribute to initiating or exacerbating inflammation in genetically predisposed hosts. A lot of work was devoted to studying the regulation of tight junction permeability through zonulin by such researchers as Fasano A.
This autoimmune disorder is known by another name-celiac disease-it is caused when a particular protein in wheat, barley, and rye triggers an immune response.
Recently, direct involvement of zonulin with celiac disease has been discovered. The ingestion of gluten induces the release of zonulin, which increases intestinal permeability, thereby stimulating the immune system in genetically susceptible individuals, thus causing inflammation, villous atrophy, and many gastrointestinal and systemic symptoms.
Some of the early work to bridge the gap between zonulin and celiac disease came from Fasano A. et al. These scientists showed that gluten is one of the more potent stimuli for zonulin release, particularly in the presence of the HLA-DQ2 or HLA-DQ8 genetic markers so commonly found in patients afflicted with the disease.
In addition, elevated levels of zonulin have been consistently found to be a feature of this disease where significant increases are seen during active disease states. These results emphasize the involvement of zonulin in the pathogenesis of celiac disease and its probable role as a biomarker for the activity and progress of the disease.
As a rapidly emerging field, the therapeutic potential of drugs targeting zonulin in celiac disease has been a matter of interest. The role of larazotide acetate, as a zonulin inhibitor, has shown to reduce intestinal permeability and improvement of symptoms in patients suffering from celiac disease.
Larazotide acetate is given to block the action of zonulin, thereby stopping the opening of tight junctions, and thus preventing loss of intestinal barrier function coupled with reduction of inflammation triggered by gluten.
Type 1 diabetes is an autoimmune destruction of the insulin-producing beta cells of the pancreas. Like celiac disease, increased intestinal permeability and zonulin are also involved in the development process of T1D.
It was found that disturbances of the zonulin pathway allow some antigens and toxins into the bloodstream, provoking the autoimmune reaction that can predispose to T1D.
It has been shown that patients with T1D exhibit higher levels of serum zonulin, primarily in the early stages of the disease.
M et al. and others demonstrated that high levels of zonulin are associated with high permeability in the gastrointestinal tract of patients with T1D and that this data supports the hypothesis that T1D pathogenesis involves zonulin-mediated gut permeability.
The relationship between zonulin and T1D points to a need to maintain the integrity of the intestinal barrier in preventing autoimmune diseases from developing. Scientific investigation into the modulation of zonulin as a potential target in the treatment of T1D is active, but its evidence on the ability to delay or halt the attack of this disease appears promising in genetically predisposed individuals by inhibiting the release of zonulin.
Increased gut permeability and chronic inflammation characterize inflammatory bowel disease, including Crohn's and ulcerative colitis.
A novel player has recently been identified in this process: zonulin, which is released with response to environmental and microbial factors that open tight junctions and consequently increase gut permeability, part of the inflammatory cascade observed in IBD.
The elevation of zonulin levels has been demonstrated in patients with IBD, particularly during acute and active phases. The correlation between serum zonulin levels and the severity of diseases may indicate that zonulin might represent a useful non-invasive biomarker in monitoring the progression of IBD.
Moreover, therapeutic interventions based on strategies that might include reducing zonulin release or blocking its action may provide novel targets for treatment in IBD.
The pathogenesis of IBD therefore initiates with the inclusion of zonulin, thereby underlining the intricate connection that exists between gut permeability and the immune system and chronic inflammation. Zonulin's function in regulating the intestinal barrier marks a specific potential target for therapeutic interventions designed to mend intestinal barrier function and induce less inflammatory conditions among patients with IBD.
Serum zonulin level measurement was proposed as a non-invasive biomarker to assess intestinal permeability. Several studies have reported enhanced serum levels of zonulin in leaky gut associated conditions, such as autoimmune diseases, metabolic disorders, and infections.
Such functions of zonulin as an intestinal barrier regulator make it very useful for understanding the mechanisms underpinning increased intestinal permeability and its contribution to disease pathology.
Theoretically, the biomarker zonulin would be useful for the early detection of leaks of diseases caused by leaky gut and monitoring the efficiency of treatments aimed at recovery of intestinal barrier function; however, the specificity and sensitivity of the biomarker zonulin remain in the ongoing research area as some studies have questioned its reliability in certain populations and disease states.
It is released in response to several stimuli, including bacterial colonization, gluten, and other environmental factors.
Bacterial toxins, such as the zonula occludens toxin isolated from the Vibrio cholerae, are known to induce the release of zonulin leading to the opening of tight junctions and consequently increased gut permeability.
This mechanism underlies the role played by the gut microbiota in regulating levels of zonulin and gut permeability.
It is mediated through activation of a cascade of intracellular signals and through the disassembly of tight junction proteins, claudins, and occludins.
These events lead to the opening of the tight junctions, macromolecule passage across the barrier, and regulation in the maintenance of gut homeostasis and preventing the onset of disease associated with increased intestinal permeability.
The genetic status may also control the release of zonulin. Some of these people will have some susceptibility to breaking down of the zonulin pathway, particularly those that have a predisposed genotype to autoimmune disorders.
Therefore, this interaction of genetics and environment will be vital in enlightening their role in the disease causation process.
Identification of zonulin as the key regulator of intestinal permeability has indicated a new field in the therapeutic intervention of diseases caused by leaky gut.
A synthetic peptide, Larazotide acetate, thereby blocks the release of zonulin, and is presently being experimented with in the context of celiac disease and other diseases caused by increased intestinal permeability.
Inhibiting zonulin prevents opening of tight junctions and keeps the functional intestinal barrier which reduces inflammation.
Besides larazotide acetate, much interest has focused on other therapeutic approaches that may modulate the activity of zonulin.
These include probiotics, prebiotics, and diet interventions leading to alterations in gut microbiota composition and reduction of zonulin secretion.
The use of zonulin inhibitors combined with these strategies could provide an integrated approach to achieving gut level restorative health and preventing disease progression accompanied by increased intestinal permeability.
Zonulin is an important modulator of intestinal permeability; it regulates the integrity of the intestinal barrier. The zonulin pathway has been incriminated as a participant in various diseases, including celiac disease, type 1 diabetes, and inflammatory bowel disease.
There is a direct correlation between higher serum levels of zonulin and increased permeability of the intestine, thus potentially aiding in the pathogenesis of all these diseases.
The determination of the concentrations of zonulin may prove to be a useful biomarker for intestinal permeability and disease activity; this is still to be worked out by specificity and sensitivity during further studies.
Therapeutic approaches toward the manipulation of zonulin release, for example, larazotide acetate, are promising in the treatment of leaky gut disorders.
It increasingly becomes clear that this pathway may be a new approach for the prevention and treatment of autoimmune and inflammatory diseases as we deepen our understanding of zonulin and its role in intestinal permeability.
Zonulin is, in fact a crucial link between the gut and the immune system, which regulating it may be the key to finding novel strategies for the treatment of wide-ranging conditions.
* Medical Disclaimer - The following information is for educational purposes only. No information provided on this website, including text, graphic, and images, are intended as substitutes for professional medical advice. Please consult with your doctor about specific medical advice pertaining to your condition(s).