Histamine Intolerance – Symptoms, Tests, and Treatments
Time to read 19 min
Time to read 19 min
Table of contents
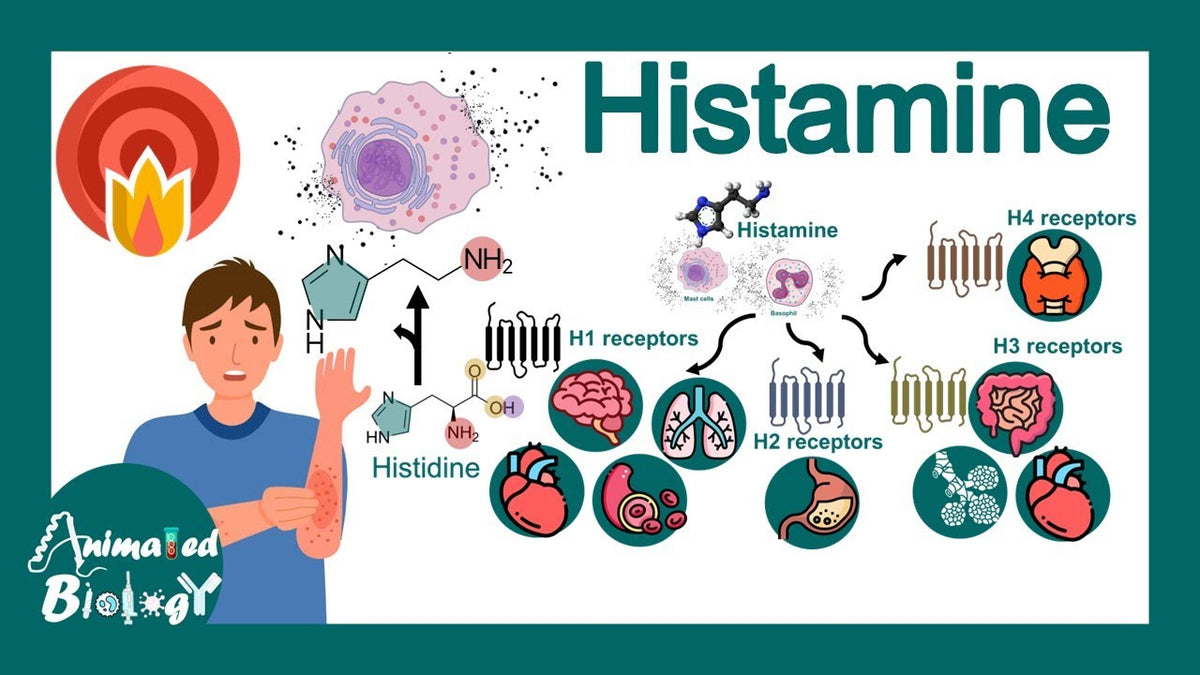
Histamine is naturally produced, a chemical compound that is created by the amino acid histidine and is produced by an enzyme known as histidine decarboxylase, which can cause issues for patients with histamine intolerance, which may include symptoms of histamine intolerance. , which may involve dao deficiency. It is stored within mast cells, basophils and in some enterochromaffin cells, it assists the immune system, regulates stomach acid, causes muscles to contract and it is also a brain chemical.
Histamine is a biogenic amine and one of several other biogenic amines which signals in the body. Although its most common use is in causing allergic reactions, it controls numerous other physiological functions, including histamine metabolism . Histamine acts by attaching to four receptor types, namely, H1, H2, H3, and H4, while also influencing serum diamine oxidase activity.
The role of histamine in the local immune response and inflammation of the body is significant, especially for those suffering from chronic spontaneous urticaria or mast cell disorders, which can also lead to gastrointestinal symptoms and other symptoms of histamine intolerance . It is stored in the tissues in an immune cell known as mast cells and basophils in the blood.
Allergic Reactions: When an immune system encounters an allergen, a non harmful substance that the immune system considers a threat and it sends large quantities of histamine.
Inflammation: Histamine causes your blood vessels to become dilated and porous, contributing to various allergy symptoms . This allows the movement of white blood cells, fluid and protective proteins to the injured or exposed area rapidly, which can trigger inflammatory reactions . The outcome is the typical symptoms of inflammation of redness, swelling, warmth and itchiness.
Defense Mechanism: Histamine facilitates the isolation of pathogens and combats them by enhancing fluid and immune cell access. The reaction may be detrimental during allergies, however with such symptoms like hives, congestion, and bronchoconstriction.
H4 Receptor: Such a receptor is mostly present on immune cells and is significant in the regulation of inflammatory diseases and autoimmune diseases.
In the digestive system, histamine plays a vital role in regulating stomach function, which involves the action of intestinal diamine oxidase .
Gastric Acid Secretion: Enterochromaffin-like cells (ECL) cells that line the stomach produce histamine.
Histamine connects to H2 receptors on parietal cells, which strongly encourages them to make and launch gastric acid (HCl), when stimulated e.g. by the hormone gastrin. It is a vital acid that is important in breaking down food and removing the pathogens ingested.
Gut Motility: Histamine also controls the smooth muscle contractions in the gut hence affecting intestinal motility.
Histamine is used in the brain as an excitatory neurotransmitter, which enhances alertness and wakefulness, and is involved in histamine catabolism . Histamine is produced by the only set of neurons located in the tuberomammillary nucleus (TMN) of the hypothalamus, which may influence blood pressure .
Wakefulness Promotion: The histaminergic neurons are the most active during the waking period and least in the nights. In binding to H1 receptors in the cortex and elsewhere, histamine stimulates and enhances the state of wakefulness.
Sedation Effect: That is why H1 antihistamines like diphenhydramine, that block H1 receptors usually make you feel sleepy, they inhibit the wake-stimulating action of histamine.
Regulation: The H3 receptors primarily play the role of autoreceptors of the histamine releasing neurons and regulate the release of histamine among other important neurotransmitters including dopamine and serotonin.
Allergy (IgE-mediated): A protein is generated by the immune system, which creates specific IgE antibodies that cause a repeatable allergic reaction, such as allergic rhinitis or conditions like celiac disease . Skin prick tests and specific IgE tests are objective tests that are typically positive.
Histamine intolerance (HIT / adverse reactions to ingested histamine): A suggested non-IgE pathology is a defective capacity to degrade histamine, frequently by way of the reduced histamine degradation capacity, intestinal DAO deficiency, or impaired methylation resulting in the histamine buildup and multi-system often unspecialized symptoms. Allergy tests are negative. The terms and specifications of diagnosis, including how to diagnose histamine intolerance, remain controversial in the specialty literature.
Feature |
Allergy (IgE-mediated) |
Histamine Intolerance (HIT) |
Underlying mechanism |
Immune system produces specific IgE antibodies to a food/environmental protein |
Impaired histamine degradation (low DAO enzyme, reduced HNMT activity, or overload of dietary histamine) |
Trigger substance |
Usually a protein allergen (e.g., peanuts, pollen, shellfish) |
Histamine itself or histamine-releasing foods |
Onset of symptoms |
Immediate to minutes after exposure |
Often delayed (30 min – several hours), cumulative load matters |
Reproducibility |
Highly reproducible with each exposure |
May vary depending on histamine load, enzyme activity, gut health |
Main systems affected |
Skin (hives, angioedema), respiratory (wheezing, rhinitis), gut (vomiting, diarrhea), cardiovascular (anaphylaxis) |
Multi-system: gut (bloating, pain, diarrhea), skin (hives, flushing), neurological (headache, insomnia), heart (palpitations, low BP) |
Severity |
Can cause life-threatening anaphylaxis |
Typically non-life-threatening, but symptoms can severely impair quality of life |
Diagnostic tests |
Positive skin prick test or serum-specific IgE |
No standardized test; possible low DAO blood activity, symptom-based diagnosis, elimination diet |
Treatment |
Strict avoidance of allergen; emergency plan with antihistamines, epinephrine |
Low-histamine diet, DAO supplements, probiotics, antihistamines (symptom relief) |
Long-term outlook |
Some allergies persist for life; others may resolve (e.g., childhood milk/egg allergy) |
Chronic, but symptoms often manageable with diet and lifestyle modifications |
Specialist |
Allergist / Immunologist |
Gastroenterologist, functional medicine, or integrative practitioner |
HIT explains that it is a clinical situation which involves accumulation of histamine in the body. This may occur either through release of histamine by the body or the consumption of foods containing histamine. When the body is unable to degrade sufficient histamine the problem occurs. The symptoms manifest both in the gastrointestinal tract, skin, cardiovascular, and nervous system. HIT is also known as adverse reactions to ingested histamine or enteral histaminosis in most studies.
Reduced intestinal DAO activity: DNAO (diamine oxidase) is the primary extracellular enzyme that decomposes histamine in the food passing through the gut. Histamine in the diet may get into the bloodstream when the levels of DAO are low.
Reduced intracellular methylation (HNMT pathway): HNMT histamine N methyltransferase employs SAMe, the methyl donor to counter histamine, particularly in the brain. Should there be a breakdown in the process of methylation e.g. the absence of SAMe due to deficiency in B-12 or floating, the activity of HNMT may be reduced.
Histamine-producing gut bacteria/dysbiosis: Some intestinal bacteria generate histamine. With the disorder of microbial balance (dysbiosis), histamine levels in the gut lumen may increase.
Drug interactions or mucosal damage: There are drugs and gastrointestinal diseases that reduce the production of DAO or disfigure the mucosal lining.
The food categories with high histamine values are fermented or polished foods, long-stored fish and meat, some cheeses and alcohol.
Histamine liberators are foods that cause histamine to release, this includes citrus fruits, nuts, and some spices although the list of foods varies depending on the source.
There are drugs that will block the enzyme DAO. These are some antidepressants, NSAIDs, opioids, as well as some anti hypertensives. Check the current lists of drugs to be sure.
Gut infections (SIBO or inflammatory bowel disease) destroy the intestinal lining and may reduce the levels of DAO.
The effect of HIT is a generalized, diffuse set of symptoms, also known as histamine intolerance symptoms . The majority of them include gastrointestinal problems and skin, respiratory, cardiovascular or neurological problems, especially when histamine intolerance occurs, and in severe cases, this can lead to histamine toxicity. . The histamine receptors are widely distributed in the body which explains the possibility of manifesting symptoms in several systems at the same time.
Gastrointestinal: bloating and abdominal distension, postprandial fullness, belly pain, diarrhea and constipation, belching, nausea/vomiting.
Dermatologic: Flushing urticaria/hives; itching; eczematous rash.
Respiratory / ENT: Congestion of the nose, sneezing; rhinorrhea; tightness of the throat.
Cardiovascular / autonomic: Palpitations, lightheadedness, hypotension in some patients.
Neurological: Headache; dizziness; lack of concentration; infrequent sleeping disturbance- due to the wakefulness effects of histamine.
Histamine also has a circadian rhythm and is what keeps us awake. Some studies indicate that histamine and mast-cell activities are at their highest in the night and the early mornings. In an investigation of rhythms that were measured daily, approximately 24 percent of patients who were suspected of having histamine intolerance (HIT) had increased daytime histamine and reduced diamine oxidase (DAO) activity compared to healthy individuals.
This implies that in some individuals, the levels of histamine and symptoms are likely to increase at specific times of the day, such as at night. These results justify the reason why individuals complain that they experience excess histamine dumps, which are sporadic exacerbation of symptoms during sleep leading to itch palpitations and awakenings.
Histamine overload can be the cause of acute or chronic urticaria. HIT must be taken into account in case of urticaria recurrence, negative allergy tests, and meal or food-related symptoms.
The diet is the key to histamine intolerance, especially when certain foods can trigger symptoms . It is not an allergy but a metabolism problem of histamine so it may make a flare up after consuming high histamine foods or foods that trigger the release of histamine. On the other hand, symptoms can be significantly minimized with the help of a low histamine diet or a histamine free diet, and maintaining a food diary can also be beneficial. .
Histamine is synthesized naturally in the fermentation process in the process of ripening, aging, and spoilage, producing various histamine metabolites . The more the food is stored or processed the greater the level of histamine is likely to be.
Fermented foods: sauerkraut, kimchi, soy sauce, miso, vinegar
Aged cheeses: parmesan, blue cheese, gouda
Cured/processed meats: salami, ham, bacon, sausages
Alcoholic beverages: red wine, champagne, beer (especially those with yeast/fermentation)
Certain fish: tuna, mackerel, sardines, anchovies (histamine rises quickly after catch if not fresh)
Vegetables: Tomatoes, spinach, eggplant, avocados (naturally higher histamine)
Other than food that contains high levels of histamine found in histamine rich foods , Certain foods that may activate mast cells to release histamine, especially certain foods. or inhibit the enzyme DAO that breaks it down, potentially leading to histamine poisoning.
To help reduce symptoms, avoid or limit:
Citrus fruits (oranges, lemons, grapefruit) → histamine liberators
Strawberries, bananas, papayas, pineapples → trigger histamine release in some people
Chocolate and cocoa products → DAO-blocking effect
Energy drinks, black tea, mate, green tea → can interfere with DAO enzyme
Vinegar-containing foods: pickles, ketchup, mayonnaise
This is not aimed at eliminating all foods, but all fresh and minimally processed foods and and monitor your own tolerance to various food intolerances.
Fresh meat (chicken, turkey, lamb) → cook and eat promptly
Freshly caught and frozen fish (cod, trout, salmon) → if frozen immediately
Eggs (fresh)
Gluten-free grains (rice, oats, quinoa, millet)
Most fresh vegetables (zucchini, carrots, broccoli, pumpkin, lettuce, cucumber)
Most fresh fruits (apples, pears, blueberries, watermelon, mango – except citrus/berries noted above)
Plant-based milk alternatives (rice milk, coconut milk, oat milk without additives)
|
Category |
High Histamine / Avoid |
Low Histamine / Safer Choices |
|
Protein |
Aged cheese, salami, tuna, mackerel, bacon |
Fresh chicken, turkey, lamb, cod, salmon (frozen immediately) |
|
Dairy |
Yogurt, kefir, parmesan, blue cheese |
Fresh cream cheese, ricotta, mozzarella (small amounts, tolerance-based) |
|
Vegetables |
Tomatoes, spinach, eggplant, avocado, sauerkraut |
Zucchini, carrots, pumpkin, cucumber, lettuce, broccoli |
|
Fruits |
Citrus, strawberries, bananas, papaya, pineapple |
Apples, pears, blueberries, watermelon, mango |
|
Drinks |
Red wine, beer, champagne, black/green tea, energy drinks |
Water, herbal teas (chamomile, rooibos, peppermint), coconut water |
|
Others |
Chocolate, vinegar, soy sauce, ketchup, fermented sauces |
Olive oil, fresh herbs, gluten-free grains (rice, oats, quinoa) |
DAO (diamine oxidase): DAO is the major extracellular enzyme which degrades dietary histaminein the gastrointestinal tract. HIT is strongly associated with low intestinal levels of DAO (genetic variations, mucosal destruction, or interaction with drugs) caused by histamine intolerance.
HNMT (histamine-N-methyltransferase): It methylates histamine in cells in the central nervous system in particular, with SAMe. HNMT activity can be reduced by genetic variants or impaired methylation including low SAMe due to B12 or folate deficiencies.
Some strains of bacteria including Morganella and Enterococcus are known to produce histamine, leading to possible dao deficiency . Dysbiosis may increase luminal histamine or and inhibit the action of dao enzymes, leading to increased histamine levels. Small studies show that individuals who experience symptoms related to food intolerances show changes in their microbiota.
SNPs in DAO and HNMT genes can influence enzyme activity.
Environmental triggers: infections, GI inflammation, certain medications, dietary patterns (high-histamine or poor food storage).
No single and universally accepted gold-standard diagnostic test of histamine intolerance (HIT). Diagnosis is now based on a close clinical history, elimination of allergies, gastrointestinal disorders, and other causes, dietary trials, and with caution, on adjunct test including DAO, plasma histamine, urinary methylhistamine, and provocation tests. Both of these tests are limited.
The most common blood test is the measurement of DAO. There is some literature of lower DAO levels correlating with symptoms, and blood sample analysis shows there is no consistency in serum DAO levels reflecting intestinal levels of DAO—the primary barrier, as cut-offs and standard assays vary. More recent appraisals indicate that DAO testing can assist in finding cases with high probability but its sensitivity and specificity are still limited as far as many patients are concerned. As an adjunct rather than as a final test.
The levels of DAO are temporary and change depending on the time of the day (circadian rhythms, meals). It may not be helpful to measure it once. The circadian profiling method will be able to expose deviations in a sub-population of patients.
New studies indicate that urinary histamine profiles and their metabolites might be valuable biomarkers but these methods remain under validation.
Other assays have been employed though the results are inconsistent and the assays are not reproducible. These are not routine tests as there are no standardized protocols as well as safe dose ranges.
There are numerous home DAO kits and so called histamine test products but not all of them are clinically valid and establish a solid basis. Take home outcomes with a grain of salt and talk to a clinician about it.
DAO enzyme activity assays (various lab brands) — reported in U/mL or HDU depending on assay.
Plasma histamine by chromatography (specialist labs).
Urine methylhistamine (H3-methylhistamine) by chromatographic methods.
Not only are there no standardized cutoffs, but there is also a lot of intra-individual variability as well as the effects of diet and medications, and poor correlation between serum DAO and intestinal DAO. The recent reviews suggest that clinical diagnosis should be backed by diet trials and that one laboratory result should not be used to form a diagnosis.
Confirm other causes are excluded (food allergy, mastocytosis, other GI disease).
Therapeutic trial of a low-histamine diet under dietitian supervision (short elimination then reintroduction).
Address underlying causes (treat gut inflammation, stop DAO-inhibiting drugs if possible, treat SIBO if present).
Consider symptomatic meds (antihistamines) and supplements (DAO enzyme orally, methylation support) where appropriate.
Antihistamines find application in the symptomatic treatment of the hives, itching, and nasal symptoms. At least there is evidence on the practice of allergy; antihistamines or enzyme supplements neither correct the underlying deficiency in DAO but can reduce symptoms.
DAOs are found as vegetal or porcine symbiotic supplements (DAOSIN(r) and others) which have been shown to have symptom relief in small, open-ended studies and pilot studies. Certain randomized trials have also shown advantages of certain conditions, such as migraine in individuals with DAO deficiency. Nevertheless, there is a dearth of large, high-quality, and double-blind-studies. DAO supplement can be used to assist certain patients, yet it is not the panacea for managing histamine properly .
Research is in early stages. Targeted probiotics are meant to decrease the histamine-producing bacteria or increase the histamine-degrading microbes. Although there is little evidence, they have encouraging results as adjunctive therapy in histamine intolerance mediated by gut.
B12, folate, B6, and SAMe are the ones that promote methylation processes that are driving HNMT. Though research demonstrates that B12 supplementation can reduce systemic histamine by aiding the process of methylation, there is a lack of solid clinical evidence. Remedying a deficiency may have a beneficial effect on some patients (see section 8).
Immediate symptom control: Take oral antihistamines when you have H 1 symptoms including oral H 1 blockers and take H 2 blockers when you experience discomfort related to acid. Emergency treatment may be required in the case of airway impairment, or anaphylaxis (rare and more characteristic of allergy than HIT).
Short term: Hydrate, avoid the suspected food trigger and take note of brief term use of antihistamines and rest. In case of symptoms recurrence, or even severity, seek emergency care.
No permanent cure is studied universally, which emphasizes the importance of treating histamine intolerance with a comprehensive approach . A combination of a personalized diet, the enhancement of the health of the gut, quitting the use of drugs that prevent the activation of the DAO, and the use of specific supplements or antihistamines can help many patients manage their symptoms effectively and prevent histamine intoxication . In cases where the root cause is temporary, e.g. damage of the mucosa, the symptoms can heal over time, and the patient can resume a normal diet; in most cases, genetic enzyme deficiencies require lifelong management.
HNMT eliminates histamine with the incorporation of a methyl group of SAMe (S-adenosylmethionine). SAMe is synthesized in the body during the methionine cycle which requires the presence of vitamin B12 and folate. Once the levels of B12 are sufficient, enough SAMe is produced in the methionine cycle because HNMT can become effective. This way, B12 status has a direct influence on the rate of breakdown of histamine, particularly within cells and the brain.
There is not much direct clinical evidence that B12 supplementation can reduce systemic histamine levels or end HIT. Mechanistic reasoning indicates that remedial B12 deficiency might benefit methylation and HNMT-broken down histamine, although it is an oblique consequence that has not been affirmed as a single intercessive medication of HIT in clinical trials. B12 is not a histamine containing foodstuff and therefore does not increase dietary histamine, making it suitable for a histamine free diet.
In case of a proven low B12 level or a methylation defect, It is plausible and possibly can improve total methylation and potentially histamine management to fix B12, talk about testing and supplementation with your practitioner, and consider maintaining a food diary. Do not think that HIT will be cured only by B12, especially when chronic intestinal symptoms are involved .
As diet and supplements dominate the management of histamine intolerance, lifestyle changes are also very significant. Poor sleep, environmental triggers and stress may also aggravate symptoms by stimulating histamine or disrupting its elimination.
Prolonged stress causes the sympathetic nervous system and may raise the level of mast cell degranulation and, as a result, trigger inflammatory reactions and histamine levels.
Mind-body practices: Yoga, meditation, deep breathing, and mindfulness exercises lower stress hormones.
Gentle movement: Low-impact workouts like walking, swimming, or stretching instead of intense exercise (which may trigger histamine release).
Nature therapy: Spending time outdoors in green spaces reduces inflammation and stress markers.
Histamine is involved in the sleep-wake cycle to make an individual stay awake. Due to improper regulation of histamine concentrations, patients usually have histamine dumps at night that may be characterized by the acute itch, palpitations, or insomnia.
Attempt to sleep and get up at the same time each day.
Avoid foods and beverages that contain high histamine and avoid alcohol at night.
Make the bedroom cool, dark, and allergen free - dust mites, mould and pet dander may cause histamine.
Before going to sleep, have some of a calming tea like chamomile or rooibos.
Nighttime symptoms are common due to natural circadian rhythms of histamine release, which interact with histamine receptors .
Light protein-rich evening meal with low-histamine foods.
Elevate head slightly during sleep (may reduce nasal congestion).
DAO supplements (if recommended by a doctor) before dinner.
Gentle stretching or relaxation techniques to calm the nervous system.
Histamine can be triggered not just by food, especially histamine rich foods, but also by environmental factors.
Allergen control: Use air purifiers, change bedding frequently, wash clothes after outdoor exposure.
Chemical avoidance: Minimize exposure to perfumes, cleaning chemicals, and smoke, which can irritate mast cells.
Temperature regulation: Both heat and sudden cold can trigger histamine release – dress in layers and avoid extreme conditions.
Eat fresh: Avoid leftovers; freeze food immediately if not eating.
Stay hydrated: Adequate water supports kidney and gut clearance of histamine.
Keep a symptom diary: Track foods, stress, and environmental triggers to identify patterns.
Plan ahead: Carry low-histamine snacks (rice cakes, pears, cucumbers) to avoid triggers when away from home.
Use antihistamines sparingly: Over-the-counter antihistamines may help, but regular reliance should be guided by a doctor.
Histamine intolerance is the inability of the organism to process histamine effectively. The immune system does not cause it as it does with allergies. Rather it is a consequence of a disproportion between what you consume the quantity of histamine that your body produces and the rate at which it is removed. Due to this asymmetry, histamine intolerance symptoms can appear and disappear, have various intensities, and resemble other health issues. In case you have symptoms that are common, intense, or have an impact on your everyday routine, you should visit a medical practitioner. Eliminating other diseases, such as allergies, mast cell disorders, and gastrointestinal diseases, they can create an individual plan to treat your symptoms.
Histamine is a chemical which is involved in the immune system, digestion and central nervous system, and can interact with exogenous histamine triggers . It is a neurotransmitter, which is critical in an inflammatory response and may be managed with the use of enzyme supplements to help manage histamine properly. . It increases blood flow, which helps the body to combat allergens and pathogens, as in the case of allergic reactions it causes itching, swelling, and mucus.
Examples of high histamine foods are old cheeses, fermented vinegar, tomatoes, spinach and eggplant, which can be particularly problematic for individuals with irritable bowel syndrome, as they are often associated with histamine. The increase of the levels of histamine in old, spoiled or fermented foods is due to the fact that the bacterial activity increases the levels of histamine, leading to elevated histamine levels which are problematic to those with histamine intolerance.
Histamine release is the rapid reaction of the body to an allergen and injurious substances. Though necessary in protection, excess histamine may lead to symptom combinations that may cause allergic reactions or inflammation.. The knowledge of its triggers will allow us to control food allergy symptoms more effectively, maintain a balance in the immunity, and decrease discomfort caused by the surplus of histamine.
Vitamin C aids in the deactivation and breakdown of histamine through increasing the enzyme diamine oxidase (DAO) which makes use of histamine. It is also a natural antihistamine which reduces the amount of histamine in the blood and helps prevent histamine intoxication. and relieves allergies. Vitamin c can help in regulating histamine when taken on a regular basis.
**Medical Disclaimer - The following information is for educational purposes only. No information provided on this website, including text, graphic, and images, are intended as substitutes for professional medical advice. Please consult with your doctor about specific medical advice pertaining to your condition(s).

