What Is Crohn's Disease?
Time to read 8 min
Time to read 8 min
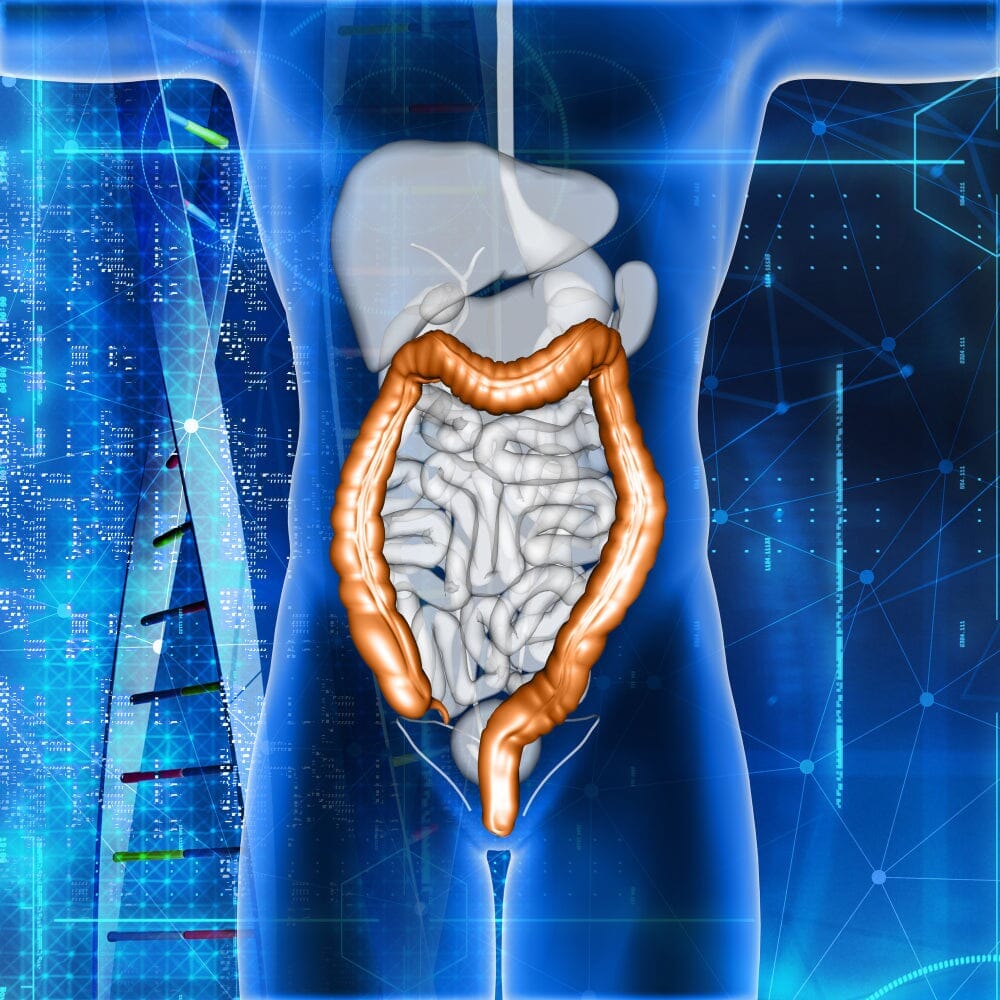
Crohn's Disease is the most common form of inflammatory bowel disease (IBD) and an inflammatory disease of the gastrointestinal tract (GI). The disease can affect any area of the GI tract from the mouth to the anus. The primary regions affected are the small bowel and the first portion of the large bowel.
Crohn's Disease may appear in patches affecting some areas of the GI tract leaving other sections completely untouched. If not treated properly, the disease can progress over the years. The more severe the disease, the faster the progression is likely to be.
Although Crohn's Disease and ulcerative colitis, another form of IBD, have many similarities and might at first glance appear to be the same disease, they are very different from each other and need to be treated accordingly.
Snippet Highlight: Crohn's Disease can be much more varied in the way it presents. As a result, the disease may be more difficult to diagnose because it can be more easily confused with other disorders. As the disease can involve any area of the GI tract, symptoms are mostly defined by which area of the digestive tract is affected.
Several studies show a high incidence and prevalence of Crohn's Disease in Western countries including USA, Canada, New Zealand, UK, Scandinavian area and Western Europe with stable increasing rate while the disease is not a common autoimmune disease among African, Asian and Eastern European countries. Recent studies indicate a considerable increase in Crohn's Disease among industrialized developing countries such as a number of Asian countries.
The results of surveys in Western countries confirm a higher rate of Crohn's Disease among female patients in comparison with male populations; while this ratio is reversed in developing countries with a low incidence rate. Moreover, people in the age group of 15-35 and 60-80 are most susceptible.
Crohn's Disease is a complex disease that results from the interaction of an individual’s genes with environmental factors and the immune system.
The following risk factors can increase the incidence of Crohn's Disease:
Crohn’s is a complex inflammatory bowel disease that over time can damage the intestines and cause symptoms such as diarrhea, gas and pain, bleeding when going to the bathroom, and the inability to eat normally. People who suffer from Crohn’s are often hesitant to talk about it.
Some common symptoms include,
Snippet Highlight: Though Crohn’s is incurable, the disease is treatable and new therapies and treatments allow most people to live normal lives. It is important not to take even what appear to be minor symptoms lightly and get checked out right away if there are frequent episodes. It is important to get early and careful diagnosis and treatment for the disease, especially because the symptoms manifest in different people very differently.
No one test can definitely diagnose someone as having Crohn's Disease with 100% certainty. The disease is diagnosed based upon a patient’s clinical history and physical examination in combination with radiologic, endoscopic, and laboratory testing. As each patient is an individual, not all patients undergo an identical evaluation; testing is tailored to each patient.
Following is a description of some of the various tests that are used in the evaluation of Crohn's Disease.
Snippet Highlight: Once Crohn's Disease has been diagnosed, the symptoms can often be effectively managed. However, the disease is chronic and changes are likely to occur over time. Symptoms may recur at times and flare-ups may develop. Patients should follow-up with the doctor to catch symptoms early and take the correct treatment.
Treatment with medication is the first therapeutic option. Treatment aims include the suppression of symptoms and the control of avoidable complications. There is no standard regimen for managing all people with Crohn's Disease. The approach to treatment must be tailored to the individual.
A perfect mix of conventional and alternative treatments with lifestyle and diet modifications can go a long way in managing the symptoms of the disorder better.
Conventional Treatments
Conventional treatment regimens have been used with varying success, such as the following approaches.
Alternative Treatments
Many studies have focused on the use of alternative treatments as potential therapeutic interventions in patients with minimal side effects. Alternative treatment strategies are limited and require extensive clinical testing before being optimized for use in patients.
Management of Crohn's Disease patients with conventional therapy is very cost-effective but with lots of side effects and remains a clinical challenge. Keeping this in mind, alternative medicine options should be explored when treating patients.
Homeopathy Treatment
Homeopathic remedies are frequently used by patients and families in the management of Crohn's Disease. Holistic treatment often gives good results through eliminating food allergies, removing toxins, parasites and fungi, replacing missing digestive enzymes and healthy intestinal bacteria, reducing inflammation, and healing intestinal lining tissues, while boosting immune function.
All of these remedies have also been used successfully for Crohn's Disease but this requires the care of a professional homeopath. He/she will find the remedies that will not only eliminate symptoms but help the body eradicate the deep patterns of weakness and susceptibility to the condition.
Ayurvedic Treatment
Ayurveda classifies most diseases predominantly based on symptoms; it categorizes Crohn's Disease under the term ‘Pravaahika’. Treatment is aimed at correcting the basic pathology of the disease, controlling symptoms or reducing complications and boosting the immune system.
Nutrition
Nutrition through intravenous supplies may be needed for Crohn’s in cases of severe weight loss, chronic diarrhea, or intestinal obstruction. Providing supplemental nutrients can be helpful in many conditions, ranging from mild to severe, and as an adjunct to drug therapy.
Research has found that many patients also have major food allergies, including problems with wheat, milk, or citrus. If the allergy is a causal factor, removing the trigger food can make a significant difference.
Overconsumption of animal fat, excess chemicals, too much of sugar, nicotine, alcohol, caffeine, chemicals and processed foods can aggravate inflammation. Eating whole foods that are primarily organic is easier on the digestive system than combined foods. Fruits, vegetables, grains, nuts, and seeds and animal products such as beef, fish, poultry, pork, and eggs are all whole foods. Organic probiotics like kefir or kombucha and consuming home-cooked food can relieve the patients from the symptoms.
Movement
Gentle exercise like walking, low-impact aerobics, Tai Chi, Qigong or yoga is suggested to increase blood flow to the digestive tract. Care should be taken not to overdo it though, as aggressive exercise could stimulate bloody diarrhea.
Exercising regularly will improve body function and health as well as attitude. It is also one of the best stress managers, relaxers and mood elevators. Another healing benefit of exercise is its positive effect on the lymph system. When people take deep breaths and move the body around gently, the lymph fluid that eliminates waste products and toxins and activates immunity is stimulated.
Yoga is a great exercise and especially good for patients with Crohn's Disease. Some natural practitioners use yoga for pain reduction which is beneficial in treating gastrointestinal disorders.
Mindset
Above all these, it is essential to keep a positive outlook so that we treat ourselves and others with the life-supporting respect and care we deserve.
Behavioral patterns are hard to break and breaking those will require discipline, work, and often guidance. The guidance can be found through a group of like-minded people in support groups.
Learning to trust yourself and the process is an important step in healing. Derive motivation for fighting the disease from your closer circle; kids, someone you love or you have to live for.
It is suggested to keep the triggers under control in the first place that can cause flare-ups as part of pain management and cure.
*Medical Disclaimer - The following information is for educational purposes only. No information provided on this website, including text, graphic, and images, are intended as substitutes for professional medical advice. Please consult with your doctor about specific medical advice pertaining to your condition(s)