Fasting vs. Non-Fasting Lipid Profile Test: Which Is More Accurate?
Time to read 16 min
Time to read 16 min
Lipid profile tests play an imperative role in assessing a person’s heart health status. These tests determine the amount of fats or lipids within the blood, and this quantification is vital as it helps determine whether the person is at a high risk of suffering from heart disease, stroke, or any other cardiovascular diseases. CVDs are one of the major global killer diseases; thus, it is crucial to monitor one's lipid values and general health.
For example, it has been the norm for patients to abstain from food a few hours before a lipid profile test, as this is thought to produce better results. However, some modern programs and the new emerging standards state that non-fasting lipid panels are as accurate in most instances. This paradigm transition has raised questions and discussions on which is best, the fasting or the non-fasting lipid profile studies, for patients and clinician providers, respectively.
This article focuses on comparing fasting and non-fasting lipid profile tests in terms of reliability, advantages, disadvantages, and application to patient outcomes. Here, we intend to present a comprehensive comparison of fasting vs. nonfasting lipid profile tests with regard to the current research, recommendations, and important considerations.
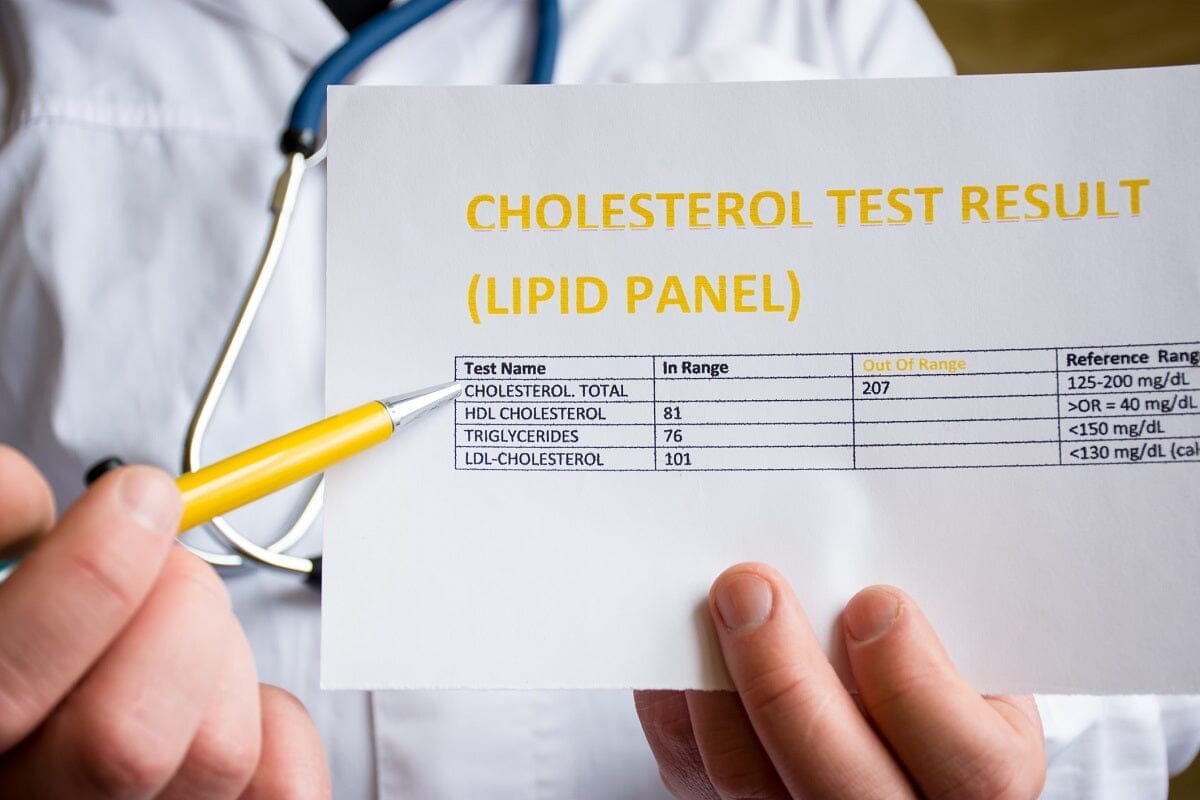
A lipid profile test is also referred to as a lipid panel and is a blood test that indicates the amounts of fats present in the blood. These lipids are essential in the proper functioning of the cell, but when present in the wrong proportion, they can result in the formation of plaques in the arteries, therefore leading to cardiovascular-related diseases.
The lipid profile typically measures four main components:
Lipid profile testing is an essential component of preventive cardiology and the management of cardiovascular disease. Hyperlipidemia and hypertriglyceridemia are major risk-associated factors with atherosclerosis, characterized by the narrowing of arteries and the development of cardiovascular diseases, such as heart attack, Strokes, and peripheral vascular diseases.
This tells the healthcare providers how much the patients are at risk of developing CVD so they can give lifestyle advice, change the patient’s diet, or even put them on medications, which can include statins, for example. This also aids in viewing patients and reviewing, in conjunction with treatments, whether they maintain optimal cholesterol and triglyceride indexes.
Getting a picture of your lipid panels might assist you and your doctor in making the right decisions regarding your cardiovascular system. Getting a test regularly is especially important for those with other risk factors for cardiovascular disease, including hypertension, diabetes, obesity, smoking, and a family history of heart disease.
A fasting lipid profile test involves the patient not taking any food or liquids for 9–12 hours prior to the test. In the course of the fast, the patient should not partake in food, drinks, or medications that may adulterate the outcome of the test. This period of fasting guarantees that the lipids being measured in the blood are not in any way affected by the intake of foods, which would give the clinician a ‘blanket ‘of the lipid profile of the patient.
To prepare for a vascular study, the patient comes in for the test, and a blood sample is taken, generally from a vein in the patient’s arm. The sample is then taken to a laboratory to determine the total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides.
Perhaps the most important reason behind fasting prior to a lipid test is the precise measurements of triglycerides. Unlike cholesterol, triglyceride level is closely related to the recent food ingestion. Later, as fats from the food consumed are metabolized, it results in an increase in the rate of triglyceride. Failure to fast gives a false impression of high triglyceride levels, thus, a wrong estimate of a patient’s baseline lipid levels.
People with high triglycerides need special tests called fasting lipid tests. These tests help doctors see exactly how high the triglycerides are. This information helps them decide the best treatment and check if it is working.
Fasting lipid tests are good because they give clear results. When a person does not eat before the test, the doctors can compare the results better. This way, they know the results are not changed by food. This is very important for people who need to keep track of their cholesterol or triglycerides over time. It helps doctors see how well treatments like medicine, diet, and exercise are working.
A key issue of controversy and concern with fasting lipid tests is the lack of patient compliance with the requirement to fast before a blood test. As much as the patients will appreciate this instruction, some might have differing health concerns, like diabetes, where they cannot go without food for 9-12 hours. Some of the patients may forget that they were supposed to fast or may even take some food or drinks at the wrong time, and hence, wrong results will be obtained, and the test has to be repeated.
Attached to time constraints, individuals with work and other responsibilities can rarely find a suitable time to fast and be subjected to the test, especially if they need to attend early morning appointments for the tests following overnight fasting.
Fasting tests are generally arranged in the morning because patients are required to fast for an amount of time overnight. That can create some issues in regard to the organization of the treatment for the patients as well as for the providers. Employees or household caretakers might not attend earlier appointments, thus delaying testing or lack of cardiovascular risk evaluation.
Further, the shortage of food can also be displeasing for them, particularly the hypertensive and diabetic patients who have to take small but frequent meals during the day. In such circumstances, one may be required to imagine the advantages of fasting lipid testing against the disadvantages and burden on the patient.
In an N-LPT, patients do not have limitations as to what they can eat or drink before the test is conducted. Contemporary versions of this type of test have become quite popular in the recent past, primarily following research showing that non-fasting lipid levels are equally useful in evaluating cardiovascular risks such as total cholesterol and LDL cholesterol.
A non-fasting test is the same as a fasting one, where a blood sample is obtained from the patient, but there are no restrictions on eating before the test. They do not need to fast; they can have their meals and even drink while they partake in this test at any time of the day.
A significant benefit of non-fasting lipid tests is the fact that they give patients a lot of convenience. This is less likely to inconvenience patients, as they do not have to rush to take the test before fasting or avoid taking it after taking a meal. This flexibility can enhance the durability of tests carried out frequently, such as lipid tests, thus enabling healthcare practitioners to continuously gauge the cardiovascular health of the patient.
Nonfasting tests are more convenient for patients with busy lifestyles, patients with children, and patients with conditions that warrant frequent eating. If the requirement of fasting is eliminated, there is a higher chance that patients will get tested more regularly, thus modifying and controlling cardiovascular disease prevention and management.
When it comes to fasting and non-fasting lipid profile tests, several studies have indicated that non-fasting lipid tests are as useful in drawing useful concentrations of the whole lipid profile, particularly the total cholesterol and the LDL cholesterol in the bloodstream. These measures are fairly consistent and are not influenced greatly by the foods recently consumed; thus, nonfasting tests are quite appropriate in most patients to evaluate their cardiovascular risk.
For example, Lewington et al.’s cross-sectional study in The Lancet showed that non-fasting LDL cholesterol is approximately 3 mg/dl higher than fasting LDL cholesterol, meaning that ‘non-fasting’ tests are valuable for most people. As a result, fasting for routine lipid testing has prompted many healthcare facilities to re-evaluate the significance of fasting, particularly when testing for LDL cholesterol and total cholesterol, which is required and not triglycerides.
Non-fasting lipid tests help lower anxiety and stress for patients. Some people feel worried about needing to fast before their medical appointments. Fasting can make them feel pressured and unsure, especially if they are not used to skipping meals.
Patients often wonder how long they need to fast and if they can drink water or other drinks. Some may even feel uncomfortable or cranky from being hungry.
When fasting is not required, patients can eat normally before their appointment. This is helpful for busy people, like parents balancing work and childcare. They can easily fit a non-fasting test into their day without worrying about meal times.
Less anxiety can also help patients take a more active role in their healthcare. When patients feel relaxed about the testing, they are more likely to keep up with health check-ups and manage their heart health.
A calm environment during medical visits can lead to better health outcomes. When patients feel supported, they may be more willing to talk about their worries and health problems. This helps build a stronger relationship with their doctors.
Non-fasting lipid tests are great for special groups, like older people, those with diabetes, and people with certain health conditions. Fasting can be hard and even risky for these individuals.
For example, older patients might need to take their medicines with food. If they skip meals, they could get low blood sugar, causing confusion or dizziness. Non-fasting tests let them eat normally while still checking their lipid levels. This is important for monitoring their heart health without fasting risks.
People with diabetes also need to watch their blood sugar closely. Fasting can cause their sugar levels to go up and down, making it hard for doctors to understand their health. Non-fasting tests let these patients eat as usual, helping keep their blood sugar steady and making it easier to schedule tests.
Additionally, people with chronic illnesses often have many medical appointments. Non-fasting tests make it easier for them to take care of their health without worrying about fasting. This helps them get tested on time, which is important for managing conditions like high cholesterol and reducing heart disease risks.
One of the major drawbacks of non-fasting lipid tests is that even though they are quite convenient and precise in some aspects, they have splendid interferences when it comes to triglyceride levels. Triglycerides have a very short recovery time and are influenced by food consumed within the shortest period, specifically fatty foods.
The levels of triglyceride triple or double within a few hours after consuming any meal, and they peak at night after dinner. Another feature that is potentially hazardous and can make it exceptionally challenging to get a correct diagnosis of first-level triglyceridemia is the post-prandial elevation of triglycerides.
Non-fasting lipid tests may not give clinicians a true picture of lipid status in patients with some conditions, including metabolic syndrome, obesity, and diabetes, where triglycerides are very significant in cardiovascular risk prognosis. However, in such scenarios, fasting tests may still be preferred since they exclude biases regarding recent meals and triglyceride levels.
However, it is also important to provide information on the specificity of non-fasting lipid tests because there are tendencies regarding misinterpretation of the results. This suggests that elevated triglyceride levels after a meal may cause an overestimation of the cardiovascular risk, especially when the doctor does not know that the patient was tested while on the meal. This may lead to further testing that is not needed or the commencement of therapy based on supposedly high triglyceride levels.
Consequently, clinicians practicing in the non-fasting lipid age are required to interpret non-fasting lipid testing, especially for patients with a previous history of high triglycerides or other lipid anomalies. The timing of the testing in relation to the last meal has to be considered, and the possible influence of various factors on the lipid levels has to be kept in mind.
In the past decade, a number of investigators have reviewed the literature analyzing the difference in efficacy between fasting and nonfasting lipid profile tests and how they correlate to potential cardiovascular events such as heart attacks and stroke.
In a definitive study of more than 300,000 participants reported in JACC: Journal of the American College of Cardiology, scientists noted that nonfasting lipid profiles are as predictive of cardiovascular threat as the conventional fasting lipid profiles.
However, there were only small differences between non-fasting total cholesterol and fasting total cholesterol (mean difference: 0.05 mmol/L; 95% CI 0.037-0.064 mmol/L), LDL cholesterol and fasting LDL cholesterol (mean difference: 0.02 mmol/L; 95% CI 0.009-0.031 mmol/L) and between non-fasting HDL cholesterol and fasting HD.
In the same way, another research study by Nordestgaard et al. revealed that non-fasting triglyceride concentrations were a significant risk indicator of cardiovascular events, which include heart attacks and strokes. This finding says we don't always need to fast for good lipid tests. It challenges the old idea that fasting is a must.
Non-fasting tests can still give important information. They show how our body uses fats after we eat. This is called postprandial lipid metabolism.
Due to accumulating evidence of NFT’s efficacy in lipid testing without the need for fasting, the majority of authoritative organizations gradually changed their recommendations. For instance, the guidelines by the American Heart Association (AHA) and the European Society of Cardiology (ESC) now endorse nonfasting lipid profiling for the majority of routine cardiovascular evaluations.
The AHA recommends the use of nonfasting lipid testing in most situations, especially with respect to total cholesterol, LDL cholesterol, and HDL cholesterol. These recommendations are based on many investigations showing that non-fasting assessments offer similar performance to fasting examinations for these critical lipid indices.
However, the AHA also urges that fasting tests could still be required for individuals with high levels of triglycerides or those within evaluation for specific disorders such as pancreatitis, which indispensably affects lipid profile because of diet's impact on triglyceride metabolism.
Likewise, the ESC has included non-fasting lipid testing in clinical practice recommendations, pointing out that non-fasting tests are easier to perform without reducing the accuracy of most lipid indicators. They also guide the clinicians in factoring in the patient’s lifestyle and, of course, their diet as they decide on the testing strategy.
The ESC also advises regular fasting tests for patients with abnormal levels of triglycerides, hypertriglyceridemia, or other patients who require quantitative assessment of triglyceride levels. This broad-spectrum approach seems to bear in mind the fact that, while several nonfasting tests make the testing process easier, some clinical circumstances require the use of fasting tests for the best treatment outcome.
Lifestyle choices are very important for our lipid levels. These choices can change the results of lipid tests. Things like what we eat, exercise, stress, and sleep can affect cholesterol and triglycerides. Knowing this helps patients and doctors make better choices.
Diet:
What we eat affects our lipid levels. Eating too much bad fat and sugar raises LDL (bad cholesterol) and triglycerides. Eating more fruits, vegetables, whole grains, and healthy fats helps lower LDL and raise HDL (good cholesterol). For example, eating a fatty meal before a test can make triglycerides higher. This can give wrong results if a non-fasting test is done soon after eating.
The choice between fasting and non-fasting lipid tests relies on each patient's status and condition, such as their general health, current lipids, and cardiovascular risk factors. In most cases, routine cardiovascular risk assessment does not require a fasting lipid profile but rather total cholesterol, LDL, and HDL cholesterol. These tests are designed to provide an overview of cardiovascular health without the additional burden of fasting.
However, there are specific scenarios where fasting lipid tests may still be recommended, such as:
High Triglyceride Levels: After any meal, they may have elevated levels of triglycerides, and therefore, the doctor may need to carry out a fasting test on such a patient to determine their true triglyceride levels. It is especially critical in patients with prior lipid disturbances and/or a predisposition to pancreatitis because postprandial triglycerides are not constant.
Family History of Hypertriglyceridemia: Some patients should undergo fasting tests due to their family history of high triglycerides or pancreatitis. It can also afford the early detection of health problems before they become major, bringing with it the opportunity for solution implementation.
Specific Conditions: Some pathophysiological states, including metabolic syndrome, diabetes, or obesity, may necessitate triglyceride testing to a higher level of precision. In consequence, fasting tests may be more suitable for these patients, as the enumerated pathologies impact lipid metabolism in a way that may distort non-fasting evaluations.
For both fasting and non-fasting lipid tests, it is important that the conditions do not change in between the tests. If a patient usually takes fasting tests, the patient should remain fasting before each test so that comparisons with previous tests can be made. This means that, as with ReP, fasting (9-12 hours) and refraining from food or drinks (other than water) prior to the test is maintained.
On the other hand, if non-fasting tests are employed, the patient should do a similar rigid routine for each of the tests. For instance, a patient of yours may normally have some tests done in the morning after breakfast, non-fast; following this tradition will help give an overview of the lipid status of the patient in the long run.
Such consistency is particularly important for those patients who require constant treatment for high cholesterol or triglyceride levels. The use of LD enables healthcare providers to monitor variations in lipid profiles to determine how changes to diet or pharmacologic intervention impact the patient’s lipid status and to make modifications to the treatment plan in response.
Fasting and non-fasting lipid tests have both good and bad sides. It’s important to understand these differences based on what each patient needs.
Fasting tests are great for getting accurate triglyceride levels. They also help create a standard way to compare lipid levels over time. This is very important for patients who have known lipid problems and need regular check-ups to see if their treatment is working.
Non-fasting tests are easier and work well for most lipid measurements. They can measure total cholesterol, LDL cholesterol, and HDL cholesterol. More research is being done, and non-fasting tests are becoming more accepted for checking heart health. This shows that it’s important for tests to be convenient and easy for patients.
For many people, non-fasting tests are a good choice for regular heart health checks. However, some people, like those with high triglycerides or certain health issues, may still need fasting tests.
In the end, patients should talk closely with their doctors to find out which lipid test is best for them. By staying informed and keeping testing conditions the same, patients can help manage their heart health. This teamwork helps patients take control of their health and work toward a healthier heart in the long run.
Non-fasting tests are often just as good as fasting tests for most cholesterol measurements.
A non-fasting lipid profile can still give useful information, but triglyceride levels might be higher.
Fasting is not usually needed for a lipid profile test, except for specific cases.
Fasting lipid panels can provide more accurate triglyceride levels, especially in certain patients.
Lipid profile tests are generally very accurate for assessing cholesterol and triglyceride levels.
* Medical Disclaimer - The following information is for educational purposes only. No information provided on this website, including text, graphics, and images, is intended as a substitute for professional medical advice. Please consult with your doctor about specific medical advice pertaining to your condition(s).









